Philips InCourage system

Vest therapy can help break the serious cycle of excess mucus, lung infections and further lung damage for people living with chronic respiratory conditions. People who use vest therapy have been shown to experience fewer pneumonias, fewer hospitalizations,1-5 and better results on pulmonary function tests,6,7 which measure how well the lungs are working.
Comfortable, effective Philips InCourage vest therapy
InCourage vest therapy is designed for easy use at home or in a clinical setting. The InCourage system works by creating percussion-like thumps to the chest, helping to loosen and thin mucus so that it can be cleared out of the lungs.
Why choose the InCourage system?
The InCourage system utilizes triangle waveform technology, which delivers a brief, intense, chest physical therapy (CPT)-like “thump” to the chest. Research has shown triangle waveform aids in clearing up to 20% more mucus than competing technology.8,9Why choose the InCourage system?
Active venting – another innovation unique to the InCourage system – immediately releases air in the vest in response to the user’s breath, allowing a deeper, more comfortable breath during therapy.Why choose the InCourage system?
RespirTech’s services support the patient at every step of the journey to better breathing.
Living, breathing proof – benefits experienced by InCourage system users
Powerful results, proven to make a difference. RespirTech’s patient outcomes program has self-reported data from thousands of bronchiectasis patients. After 12 months of Philips InCourage vest therapy paired with RespirTech’s support program, user data showed9 10

Yearly rate of hospitalization decreased

62%

Ability to clear lungs
Good-excellent rating increased

63%

Respiratory health
Good-excellent rating increased

46%

Antibiotic use decreased

13%
Get to know the InCourage system – designed with you in mind

Machine washable vest
Machine wash and dry without disassembly
Quickfit sizing vest
Set tabs at first use for a repeatable fit without need for adjustments
Self-locking hoses
Connects ports securely to unit and vest - levers grab and lock hoses into place for a secure connection
User-friendly control panel
One-button start and simple programming for a wide range of therapy options
Comfort and style for patients of all ages and sizes
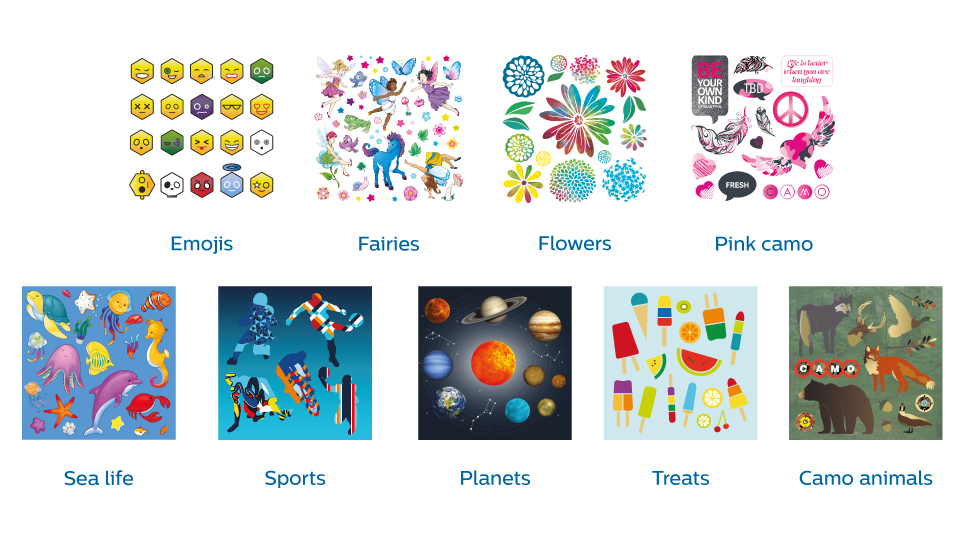
Philips InCourage comfort vests offer a personalized fit through a wide range of sizes (from 16”-60”) and the use of adjustable straps. Users can also show their individual style with the system’s colorful patterned vest fabrics and unit decals.
Vibrant vest patterns

Colorful decals for your device

Philips ClearChest comfort vests and bands for hospitals
In clinical settings, the InCourage system is used with ClearChest hospital products. Developed in collaboration with ICU and critical care professionals, these single-use vests, bands and disposable hoses minimize the risk of cross-contamination.
The clear choice for acute and long-term respiratory care

ClearChest comfort band

ClearChest upper lobe comfort band

Roll stand and accessories

ClearChest comfort vest
Disposable hoses
- How does the Philips InCourage system work?
- How to use the InCourage system quick start function
- How to clean the InCourage system
We’re here to help
We’re dedicated to helping patients benefit from our devices. RespirTech’s licensed respiratory therapists and registered nurses visit patients and caregivers at home to deliver personalized training sessions. We follow up with check-in calls to monitor progress. In case of technical issues or questions, support staff are available by phone from 8 a.m. to 5 p.m. CT, Monday-Friday at 800.793.1261.
I was on antibiotics every month for the last 40 years. I’ve used the InCourage system for over two years [and] I haven’t had to take antibiotics.* I have so much more energy, more of the desire to want to do things. It’s completely changed my life.”
– Marjorie M., CA, bronchiectasis patient
*Individual results may vary
References
2. Overgaard PM, Radford PJ. High-frequency chest wall oscillation improves outcomes in children with cerebral palsy. CHEST 2005; 128 (4): 354S. Note: A retrospective quality assurance review on 13 children with cerebral palsy. 3. Plioplys AV, Lewis S, Kasnicka I. Pulmonary vest therapy in pediatric long-term care. J Am Med Dir Assoc 2002;3:318-321. Note: Study of 7 quadriplegic cerebral palsy patients, 4 having epilepsy. 4. Lechtzin N, Wolfe LF, Frick KD. The Impact of High-Frequency Chest Wall Oscillation on Healthcare Use in Patients with Neuromuscular Diseases. Annals of the American Thoracic Society 2016;13(6):904-909. Note: 426 patients NMD patients. 5. Barto T, et al. Registry Outcomes for HFCWO Vest Therapy in Adult Patients with Bronchiectasis. Poster presented at: Am Thor Soc Intern Confer; 15 May 2016; San Francisco, Calif. Note: 2596 BE patient registry study comparing hospitalizations, antibiotic use and self-reported QOL metrics before and after HFCWO therapy. 6. Warwick WJ, Hansen LG. The long-term effect of high-frequency chest compression therapy on pulmonary complications of cystic fibrosis. Pediatr Pulmonal 1991; 11:265-271. Note: 16 CF patient study comparing pulmonary function following CPT to HFCC therapy. 7. Arens R, Gozal D, Omlin KJ, Vega J, Boyd KP, Keens TG, Woo MS. Comparison of high-frequency chest compression and conventional chest physiotherapy in hospitalized patients with cystic fibrosis. Am J Repir Crit Care Med 1994; 150: 1154-1157. Note: 50 CF patient study comparing conventional CPT to HFCC. 8. Milla CE, Hansen LG, Weber A, Warwick WJ. High-Frequency chest compression: effect of the third generation compression waveform. Biomed Instrum Technol 2004; 38:322-328. Note: 8 CF patient study comparing triangular vs. sine waveform technology. 9. Kempainen RR, Williams CB, Hazelwood A, Rubin BK, Milla CE. Comparison of high-frequency chest wall oscillation with differing waveforms for airway clearance in cystic fibrosis. Chest. 2007;132(4):1227-1232. 11. Methodology: Phone surveys at regular intervals with bronchiectasis patients using the InCourage system. Data collection began 10/01/2013. As of 05/31/2021, the total cohort was 23,213 patients; 21,049 patients completed the baseline survey; 13,303 patients in 1-month cohort; 9,569 in 6-month cohort; 7,720 in 12-month cohort
1. Giarraffa P, Berger KI, Chaikin AA, Axelrod FB, Davey C, Becker B. Assessing efficacy of high-frequency chest wall oscillation in patients with familial dysautonomia. CHEST 2005;128:3377-3381. Note: Year-long study of 15 patients with pulmonary disease due to Riley-Day syndrome.
10. RespirTech’s bronchiectasis patient outcomes program consists of follow-up calls at periodic intervals for up to two years to encourage HFCWO adherence and ensure the device is properly set for individual needs.







